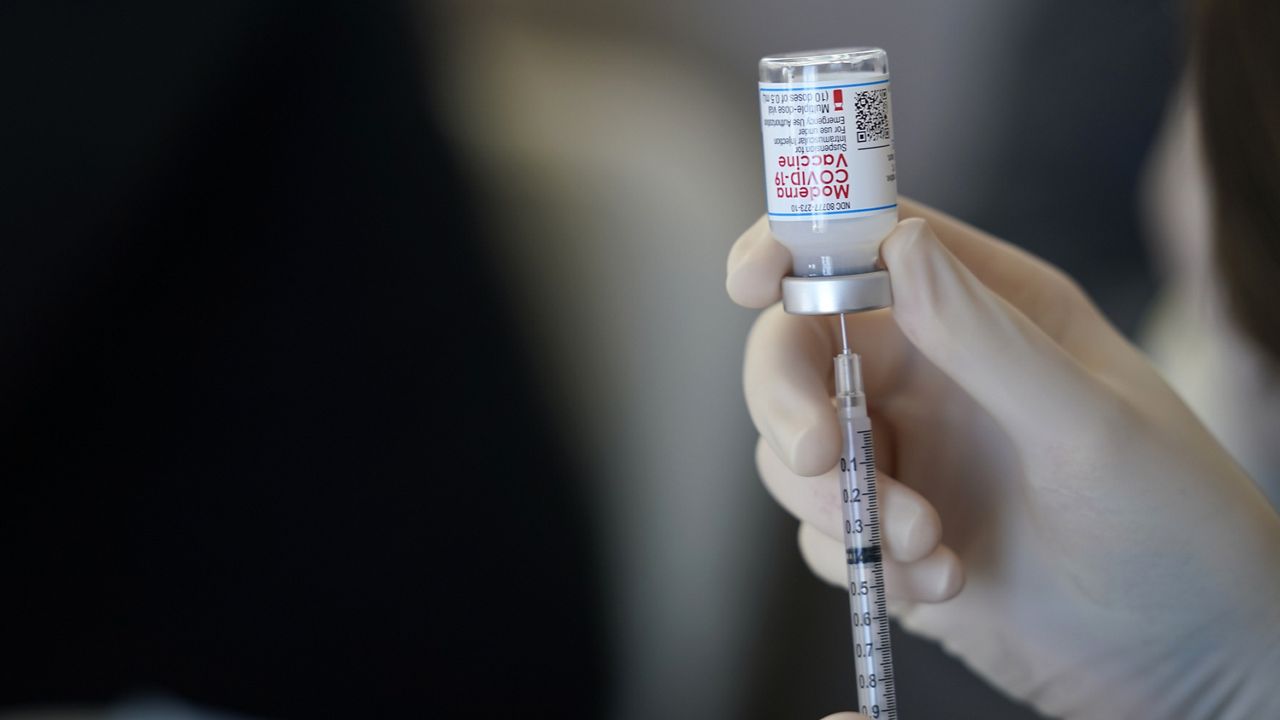
The National Institutes of Health (NIH) is launching a study about why some people have experienced allergic reactions to the COVID-19 vaccines developed by Pfizer-BioNTech and Moderna.
"The public understandably has been concerned about reports of rare, severe allergic reactions to the Moderna and Pfizer-BioNTech COVID-19 vaccines," said Dr. Anthony Fauci, the nation's top infectious disease expert and the director of the National Institute of Allergy and Infectious Diseases (NIAID).
Some people have reported allergic reactions to the vaccines, including severe reactions known as anaphylaxis. Health officials say that severe reactions are rare, and most have occured in people who have a history of allergies.
"The information gathered during this trial will help doctors advise people who are highly allergic or have a mast cell disorder about the risks and benefits of receiving these two vaccines," Dr. Fauci added. "However, for most people, the benefits of COVID-19 vaccination far outweigh the risks."
The study will enroll 3,400 participants, between ages 18-69; 60% will have "either a history of severe allergic reactions or a diagnosis of a mast cell disorder," while 40% will not. Some participants will receive some combination of the Pfizer-BioNTech vaccine, the Moderna vaccine, or a placebo, but by the end of the trial, all participants will receive a full two-dose course of either vaccine.
"A systemic allergic reaction to a vaccine occurs in one or more parts of the body beyond the injection site," the NIH said in a release announcing the study. "If such an allergic reaction occurs in study participants, investigators will assess whether the reactions are more frequent in participants who are highly allergic or have a mast cell disorder than in participants with no allergic history. In addition, investigators will examine the biological mechanism behind the reactions and whether a genetic pattern or other factors can predict who is at most risk."
Allergic reactions are rare, but possible, medical experts say. The U.S. is seeing allergic reactions at a rate of 11.1 per 1 million doses, according to data from January.
An immediate allergic reaction typically happens within 4 hours of receiving the vaccine, according to the Centers for Disease Control and Prevention (CDC), and symptoms can include hives, swelling, and wheezing.
"Symptoms of anaphylaxis often occur within 15-30 minutes of vaccination, though it can sometimes take several hours for symptoms to appear," the CDC says. "Early signs of anaphylaxis can resemble a mild allergic reaction, and it is often difficult to predict whether initial, mild symptoms will progress to become an anaphylactic reaction. In addition, symptoms of anaphylaxis might be more difficult to recognize in people with communication difficulties, such as long-term care facility residents with cognitive impairment, those with neurologic disease, or those taking medications that can cause sedation."
The CDC recommends 15 minutes of observation post-shot for most people, but 30 minutes for people with a history of immediate allergic reaction to another vaccine or injectable therapy.
The results of the trial are expected later in the summer.