This story is the second installment of our three-part series on the country’s diabetes epidemic.
NEW YORK – Around one in five American adults visit an emergency room each year. They’re typically seeking care for an urgent health problem. But these moments of contact with the health care system create opportunities to discover other underlying, undiagnosed issues.
For instance, at New York University’s hospitals, it’s required for emergency room nurses to offer HIV screening to each patient who walks through their doors.
Dr. Reed Caldwell, the Chief of Service at NYU Langone Perelman Emergency Department, saw an opportunity to look for another insidious disease — one that often goes undiagnosed for far too long.
“In the communities that we serve, the threat of diabetes, prediabetes, is actually more than the threat of HIV presently,” he says. “So I started to think of ways that we could build diabetes screening into the care of our patients.”
Four years ago, one of NYU’s Brooklyn hospitals started offering emergency room patients the A1C blood test. The test, which measures blood sugar, is used to diagnose diabetes.

Caldwell is most concerned about patients who are at high risk for type 2 diabetes. “Patients over 35 years old, patients with a BMI over 25 and patients that don't have any history of diabetes or prediabetes, those are the patients that flag for us to screen.”
Caldwell’s suspicions were confirmed — 40 to 50 percent of the patients screened were positive for prediabetes or diabetes.
Before the pandemic, the number of people diagnosed with diabetes nationwide had doubled over the previous 20 years — and the coronavirus has made matters worse. Experts don’t understand why, but new research shows that past COVID-19 infections are leading some people to develop diabetes. The need for early interventions, doctors say, is more urgent than ever.
“We need to keep working harder and we need to find people and we need to take great care of them,” Dr. Caldwell says.
NYU’s screening program has since expanded to several more of its emergency departments throughout the New York City area. When a patient tests positive for pre-diabetes or diabetes, they’re then linked to a provider who can help them manage it.
“A huge part of this has been that linkage to care and helping people find a primary care doctor or a health home,” Caldwell says.
But this type of screening isn’t yet standard practice around the country — and it’s just the first step. Avoiding or reversing full-blown type 2 diabetes is no small feat; it requires a complete lifestyle change.
“They need regular check-ins. They need a lot of education around the different pillars of lifestyle change,” says Dr. Michelle McMacken, the executive director of nutrition and lifestyle medicine at NYC Health + Hospitals. “Let's face it, it doesn't come easily in our society. People need to understand, how do I work with my family around this? What happens if I go to a party or out to dinner? What happens when it's too cold to exercise outside?”
In 2019, at Bellevue Hospital, a government-run facility in New York City, McMacken helped launch a plant-based medicine program to better support patients with diabetes, pre-diabetes and other chronic conditions.
“A suboptimal diet is actually the number one risk factor for dying of a chronic disease. It dominates everything else. The evidence is so strong around eating a plant based or mostly plant based diet for reducing risk,” she says.
Patients in the program are offered cooking classes and work with doctors, dieticians, health coaches and support groups to make lasting changes to their diets and daily habits.
“If it's a relatively new diagnosis of type two diabetes and people make intensive lifestyle changes, we have great science to show that many of them can go into remission,” she explains.
“This program, for me, has been like the wheel that keeps me moving forward, this team of people that are involved in this,” says Glenis Torres, a patient who went through Bellevue’s program.
Torres was first diagnosed with pre-diabetes in her native Dominican Republic.
After moving to the U-S three years ago, she found out she was diabetic.
Before enrolling in Bellevue’s program, all her previous efforts to change her habits didn’t stick. Those efforts included a program based on payments for following a diet and exercise program.

“You only received money. It didn’t give me any lessons like this program,” Torres says. “It only worked for me while I was getting the money, and until I finished the program. But after, I gained the weight back, and my diabetes went up."
During the pandemic, Torres’ health declined further as the family spent a lot of time stuck at home, watching TV and snacking.
Torres’ daughter, Yamile Santana, says, “We all gained weight. We weren’t going out.”
Torres became increasingly worried about her health, particularly as she learned how pre-existing conditions like diabetes can lead to worse outcomes with COVID-19.
“Many people died. And diabetes puts people more at risk. That impacted me, it impacted me a lot,” she says.
She also simply wanted to feel better.
“I was living the life of an 80 or 90-year old. I was always tired. I never wanted to go out. I always wanted to sleep. So I said, I’m too young for that. I have a two-year-old grandson and I need energy,” Torres explains.
McMacken says finding this kind of personal motivation is crucial to staying on track over the course of the lifestyle medicine program.
“Usually we set sort of an action plan moving forward. What's your why? What's your reason for being here?” says McMacken. “We identify what that why is really early on so that we can use that as an anchor as the patient goes through the program.”
Seven months after starting the program, Torres has seen a real transformation. She’s lost nearly 20 pounds, decreased her blood sugar, and improved her mood.
“Before, I was tired, depressed, sad, in a bad mood, and now I have energy to attend to my grandson, to do my thing,” she says.
Now, Torres is in the habit of preparing healthy plant-based meals for herself — swapping meat with tofu, white rice with brown, and adding plenty of veggies. She’s also changed her relationship with food.

“Food is my ally,” Torres explains. “It’s what gives me energy, it’s what gives me health.”
Torres still enjoys some Dominican favorites, like rice and beans, but she’s learned how to prepare them in healthier ways.
“I have added, for example, more yellow and red colors to my plate, which give me fiber and vitamins. I make brown rice with multi-colored quinoa.”
Podcast
Erin Billups joined Spectrum News NY1's Errol Louis' podcast "You Decide with Errol Louis" to discuss their new collaborative special report “USA1C: Fighting the Rise of Diabetes,” which is currently airing on Spectrum News nationally.
Dr. McMacken says a key component of the lifestyle medicine program is helping patients incorporate the foods they already eat into their new diets.
“I think that it is really important that we honor and celebrate cultural traditions,” she says. “Many healthy foods are often part of those cultural traditions and can be put at the center of the plate.“
Torres sees the need for broadening education and access to healthier foods in her community.
“Spanish speakers, Black people, we think that eating healthy is not for us, because we come with the custom of eating differently, of eating fried food,” she explains.
Recently, during a trip to a health food store, she had a disheartening experience after asking a Spanish-speaking employee for help finding ingredients.
“She said, ‘No honey, don’t look for that here. This supermarket isn’t for us, it’s for white people.’ I felt sad.”
Black and Brown communities experience the highest burden of diabetes, partly because there are fewer options for healthier food, and partly because supportive lifestyle medicine programs like Bellevue’s are not widely available. In these neighborhoods, diabetes can sometimes feel inevitable.
“There’s this tragic normalization of it where you’ll hear people just in conversation on the block or in church talking about, ‘oh, my sugar’s acting up’ as if it was a sprained ankle or something like that. You want to try to intervene in the conversation and tell people it doesn't have to be this way,” says Spectrum News political anchor Errol Louis, a co-reporter on this series.
When it comes to policy change, Louis says, there’s often a leadership void.
“There's no substitute for somebody, whether it's a governor or a mayor, a political leader of some kind, stepping forward and saying this is what we're going to do and this is why we're going to do it,” Louis explains.
One remarkable transformation is a very public one in New York City — that of New York’s current mayor, Eric Adams. Six years ago, Adams received a diabetes diagnosis. He was losing sight in one of his eyes and experiencing tingling in his fingers and toes. Adams took matters into his own hands.
“He switched to a plant-based diet and within two months had dropped, I think 35 pounds, within six months had reversed the diagnosis,” explains Louis. “And he's been an evangelist ever since for a different lifestyle.”
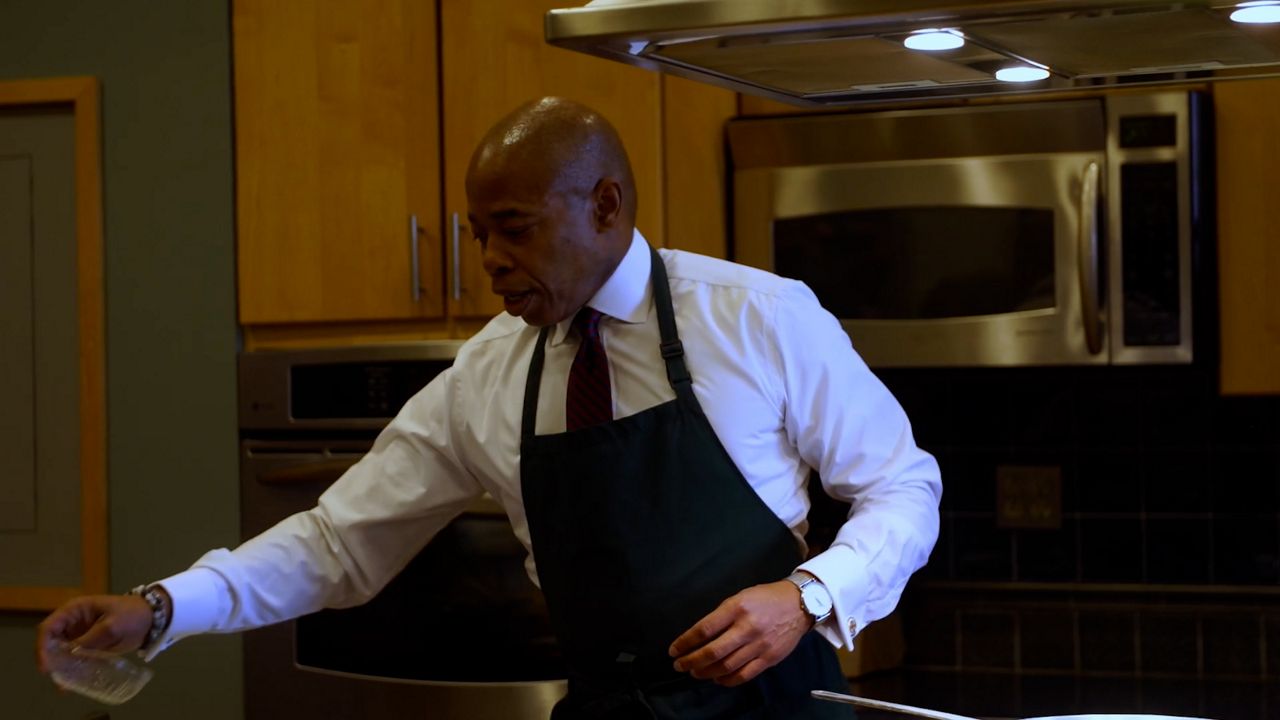
A longtime advocate for systemic change in health care, the mayor is making Bellevue’s plant-based medicine program available at six more sites, with Dr. Michelle McMacken leading the program.
“These evidence-based lifestyle behaviors can have a huge impact, not just on preventing and reducing the risk of chronic diseases, but actually treating these conditions and in some cases, actually turning things around. Just as Mayor Adams did,” McMacken said at a press event announcing the program earlier this year.
“We have a mayor who was struck with diabetes, who happened to take this particular course of action, who now believes that he can sort of bring it to scale and use it as public policy. You needed all three of those things to happen at the same time as you have a budget that can accommodate it,” Louis explains.
Nationwide, the CDC estimates the annual cost of diagnosed diabetes is more than $300 billion. Added to this is the emotional cost for the patients living with chronic illness — and for those caring for them. Adams and McMacken hope New York’s program can serve as a model for how public dollars can be better spent to fix the crisis.
“It’s not how much it costs for this program,” Adams said at the press event. “[It’s] how much is it going to cost us if we don't have this program. Our healthcare system is not sustainable.”
“We are trailblazing here,” says McMacken. “What I would like to see is really for this to be a household concept, in the medical home and in people's homes.”
For more, watch Part 1 and Part 3 of Erin Billups’ and Errol Louis’ joint series on the nationwide diabetes crisis.



